7 Reasons Why The Roof Of Your Mouth Hurts When Swallowing


Do you ever find the roof of your mouth hurts when swallowing? Most of us probably don’t give as much thought to the roof of our mouth as we might our teeth, tongue, or cheeks. But when something is wrong with the roof of our mouth or it hurts, there’s pretty much no way to ignore it. You’re going to feel it every time you’re talking, drinking, or eating.
The roof of our mouth is made up of two parts: the hard palate and the soft palate. The hard palate makes up the bulk of it and is reinforced by the bone in the roof of our mouth. The soft palate is the portion furthest back, closest to our tonsils, and is looser tissue due to the movement needed for swallowing. The roof of mouth hurts when swallowing depending on which part of our palate is involved.
Why Does My Palate Hurt When Swallowing
Anytime our roof of mouth hurts when swallowing, there are some common causes that you’ll want to rule out. In fact, they’re probably some of the first things your dentist or dental hygienist will ask you about.
Want more dental health news and tips from TTG? Sign up for our weekly newsletter.
1) Trauma, Injury, Or Burn
Treatment
Time and a modified diet. Avoid anything that’s hot or hard/crunchy for at least a few days. Stick to softer foods instead. You don’t want to re-burn or re-traumatize the same site again or it will just take longer to heal.
2) Smoking Or Vaping
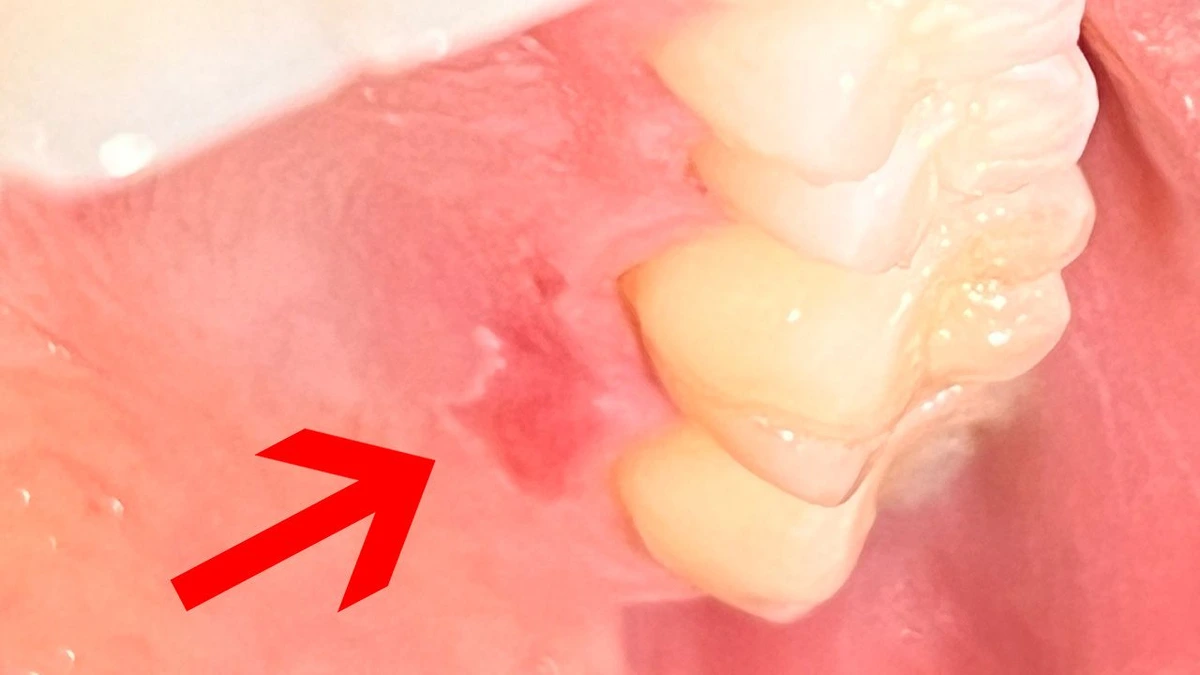
Any time we inhale something where high temperatures are involved, it can cause physical changes to the oral tissues that line the roof of our mouth. Tobacco stomatitis usually looks like whiter-colored tissues with tiny red pinpricks scattered across it. Typically, it’s somewhere in the middle or further back on our hard palate due to where steam or smoke first hits when we’re inhaling something. You can see this type of scenario with all types of inhalants, including recreational drugs or vaping devices.
Treatment
The only way to get your mouth to heal in this scenario is to stop smoking or vaping. A tobacco cessation plan can help you to reasonably set goals and cut back on how much of the inhalant product you’re using. If you’ve been looking for a reason to kick the habit, this is your sign.
3) A Yeast Infection
Oral thrush — which is common in elderly, infants, and immunocompromised individuals — is a type of yeast infection. It can create a red, raw surface on various tissues throughout your mouth (including your palate.) At other times, you’ll see a thin, white, cottage-cheese-like residue. If you were to wipe it off, there would likely be raw, red tissue underneath it. Most people with oral thrush also experience at least some mild symptoms of bad breath.
Treatment
Your dentist may need to prescribe a steroid cream or anti-fungal medication to use at home each day. Other things that can help include eating yogurt, taking probiotics, and of course re-vamping your oral hygiene routine. You’ll probably want to consider tossing or sterilizing your current toothbrush head to make sure you’re not re-infecting your mouth with the same bacteria every day.
4) Denture Stomatitis
If you’re a denture (or partial denture) wearer who finds that the roof of mouth hurts when swallowing, you might have a common condition called denture stomatitis. Symptoms often include burning, red tissues in the roof of your mouth. They’re most noticeable when you take your denture out and your palate finally comes into contact with your tongue or toothbrush. Denture stomatitis is similar to the above-mentioned yeast infection and is caused by a buildup of bacteria underneath your prosthesis. Usually, it’s due to wearing your denture overnight or not cleaning it well enough. It can be aggravated by a prosthesis that rubs or doesn’t fit well.
Treatment
Make sure you’re removing your prosthesis nightly. Never. Never. Ever sleep in your denture or partial overnight. When you take it out, soak it in an effervescent denture cleanser and lukewarm water. Clean the inside of your mouth with a soft, damp washcloth. A lukewarm saltwater rinse is also helpful. The next morning, remove your denture from the solution and brush it thoroughly, then rinse it again with tap water. Clean your mouth one more time before putting your denture back in. If symptoms are moderate to severe, your dentist may need to prescribe an anti-fungal medication or steroid cream.
5) Strep Throat
If you have a really severe case of strep throat, you might find that it hurts to eat. In this case if the roof of mouth hurts when swallowing, it’s probably your soft palate that’s sore (or you’re getting some type of referred pain.) Since your soft palate butts up to your tonsils, it’s common to feel some discomfort any time the back of your throat is really sore or infected. If you open wide and look in the mirror, you’ll probably see a patchwork of red and white around your tonsils. The redness will probably also have spread into the tissues around them, including your palate.
Treatment
Strep throat is a bacterial infection that, if not treated, can progress into more serious infections such as scarlet fever. Most treatments include a basic course of antibiotic therapy. It’s also important that you change out your toothbrush to avoid re-infecting your mouth with the same bacteria. Rinsing with a lukewarm saltwater solution a few times a day also helps. Some physicians will also recommend a tonsillectomy if you suffer from repetitive infections.
6) Tonsillitis
Chronic tonsillitis isn’t the same thing as strep throat, but a lot of the symptoms feel the same. Sore throat, the roof of mouth hurts when swallowing, or redness and irritation are typical. It’s common to see deep pits or “craters” in the surface of your swollen tonsils. Some people even get tonsil stones (tonsilloliths) due to bacteria calcifying inside of those small tonsillar crypts. A lot of the time people can have tonsillitis without any other symptoms of infection, like fever or fatigue. However, they may see a correlation between flare-ups and chronic allergies.
Treatment
If tonsillitis symptoms are caused by allergies, your physician or allergist will likely place you on a daily medication for preventative purposes. Chronic tonsillitis that isn’t controllable with home care or lifestyle changes is usually treated with a surgical tonsillectomy. Especially if recurring strep throat infections are also present.
7) Epiglottitis
Your epiglottis probably doesn’t get as much attention as your tonsils or tongue do, but it’s just as important when it comes to eating and swallowing. The epiglottis is that small flap of tissue just behind your tongue that helps block off your windpipe when you’re swallowing food. This is one of those times where referred pain can come into play. By referred pain we mean that something adjacent to what’s actually infected/hurting also feels sore. Your brain may not be able to tell exactly which part of your mouth it’s coming from. We see referred pain in teeth all of the time. In this case if your epiglottis is irritated, swollen, or infected, it can make the entire back of your mouth hurt (including the roof of your mouth.) But with epiglottitis, you’ll probably see additional symptoms of changes in your voice, drooling, or difficulty swallowing.
Treatment
Treatment for epiglottitis may be more aggressive since it can restrict your breathing. Without treatment it can, unfortunately, be life threatening. In rare situations it can even require intubation. Medication is usually a must.
Home Remedies
Any time you have a sore somewhere in your mouth, you want to focus on keeping your mouth clean and alleviating the inflammation. If there’s an infection or tenderness that lasts more than two weeks, you need to seek out professional care. All of that being said, if you’re exhibiting short-term symptoms, here are some safe at-home remedies to try to ease the discomfort.
Anti-inflammatories
Inflammation is one of the biggest sources of pain, especially inside of our mouth. Non-steroidal-anti-inflammatory medications (NSAIDs) like ibuprofen or Motrin work best for treating swelling. Always take them as directed. You can also alternate ibuprofen with acetaminophen (Tylenol) for a pain relief/anti-inflammation combo.
Taking Antacids
Antacids can provide relief if the pain is related to some type of gastrointestinal disorder or heartburn, making it easier to rule out the cause of your symptoms. Some people will actually mix antacids like milk of magnesia with other ingredients to create what’s called a “miracle mouthwash.” They gargle with it and the antacid helps to coat the sensitive tissues in your mouth for temporary pain relief.
Gargling with Salt Water
Saltwater is a convenient, cheap, and effective way to manage oral inflammation and irritation. Whether you just had oral surgery or are getting over strep throat, rinsing with it a few times a day can help to naturally draw out swelling for some gentle pain relief. For the right ratio, use one teaspoon of table salt with an 8 oz. glass of slightly warm tap water. Stir it until completely diluted.
Avoid Alcohol and Tobacco
Anything tobacco or vaping related should be avoided. The steam and high temperatures from inhalants will pose a constant irritant to your mouth. Even smokeless tobacco has tiny particles inside of it that can delay wound healing. As far as alcohol goes, take a break from any adult beverages as well as over-the-counter mouth rinse that has alcohol listed as an ingredient.
When To See A Doctor
Ok. This is one of those times where we have to have scary conversations about things that could potentially be life-threatening. In this case, it’s oral cancer.
Oral infections such as thrush or stomatitis can also be addressed by your dentist. Since they’re familiar with a wide range of oral diseases and infections, dentists can typically diagnose the condition without having to run extra labs or take a biopsy.
Your dentist is the best practitioner to see when you have something going on inside of your mouth, simply because they’re more familiar with the oral cavity than most other types of medical professionals. Or if you already have a relationship with an oral surgeon, they can perform an exam as well. The important part is to rule out anything serious as early as possible.
Overview
There are tons of reasons why you might find the roof of mouth hurts when swallowing, eating, or talking. Usually, it’s going to be something related to your diet, lifestyle habits, oral hygiene, or an infection. But it can also be a serious condition that you’ll need to see your dentist about. If home care and natural remedies don’t ease your symptoms within two weeks, it’s time to go ahead and see a professional for a more detailed examination.
Make your inbox smile!
Subscribe